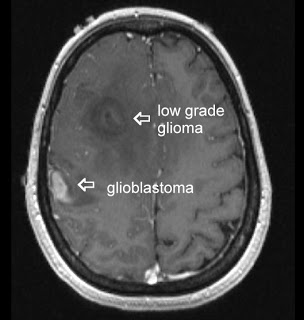
Glioblastoma multiforme (GBM) are malignant brain tumors, classified by the World Health Organization (WHO), as grade IV tumors of neuroepithelial tissue and are the most common and deadly intracranial tumors, accounting for more than 70% of all brain tumors. The current course of GBM treatment entails surgical resection followed by administration of radiation and chemotherapy. However, despite this aggressive regimen and their devastating side effects on the patient, there are several obstacles that hinder their effectiveness; surgical resection of the primary tumor leads to injury to the surrounding normal tissue, while chemotherapy and radiotherapy cause toxicity to the healthy tissue in the brain. Furthermore, some anatomical feature unique to the central nervous system (CNS) such as the blood brain barrier (BBB) and the densely packed structure of brain’s parenchyma inhibits effective drug delivery throughout the brain.
Despite improvements in surgical techniques and post-operational delivery of chemotherapeutics and radiation, the prognosis for GBM patients remains dismal, making these lethal tumors virtually incurable. One of the most prominent intrinsic behaviors of GBM is its invasiveness, such that single glioma cells travel a distance from the tumor mass and invade adjacent brain tissue. Due to the inherent capability for malignant glioma cells to rapidly proliferate and metastasize away from the primary tumor mass, surgical resection of the tumor is almost always followed by tumor recurrence (rGBM) with foci located as close as 1 centimeter from the resection cavity or as far as the opposite hemisphere. Although the history of glioma treatment dates back to the 19th century, the median survival of patients remains less than 14 months post-diagnosis.
Approximately two-third of rGBM patients are incapable of enduring additional surgical resections. Thus, for over 2 decades, Laser interstitial thermal therapy (LITT) has been used for extirpation of several malignant tumors, especially for patients with rGBM. LITT refers to utilization of low-powered thermal energy to locally cytoreduce the tumor tissue through transdermal thermocoagulation. Nonetheless, a number of technical barriers of the LITT device have impeded its widespread efficacy; two of these major barriers include lack of real-time monitoring of the tissue during treatment, as well as the control of the LITT energy (wavelength) output to correspond with the real time status of the brain tissue (healthy vs. tumor).

In a recent study published in the Journal of Neurosurgery, Andrew Sloan’s group (Monteris® Medical) reported their results from the First-In-Man (FIM) Phase I clinical trial of their NeuroBlate™ Thermal Therapy System (also know as AutoLITT), which consists laser treatment of recurrent/progressive brain tumors in combination with intraoperative magnetic resonance imaging (MRI) technology. This system overcomes some of the major obstacles to LITT; without the use of radiation, it employs high-resolution MRI images of the brain in real time, which allows surgeons to visualize the progress of tumor ablation at all times, thus directing and controlling the laser deposition to increase treatment efficacy and minimizing harm to the surrounding healthy tissue.
The FDA has designated NeuroBlate™ Thermal Therapy System as safe, since no severe clinical toxicity or procedure-related neurological deficits were caused by this system. This Safety Trial was conducted on 10 patients (median age 55) with recurrent or progressive GBM in whom standard radiotherapy with or without chemotherapy had failed. Based on this study, not only NeuroBlate treatment did not cause any adverse side effects in the subjects, but it also resulted in higher response and survival times than expected.
The technological advancements of NeuroBlate™ Thermal Therapy System which allow a minimally-invasive, and possibly safer method of performing resections, not only for GBM, but perhaps also utilized for the future surgical resection of other cancers. Nonetheless, further investigation is needed to optimize NeuroBlate™ Thermal Therapy System in increasing the mean percentage of treated tumor at the intent-to-treat dose, and determine the long-term efficacy of this system compared with traditional surgical resection.
Further Reading:
Results of the NeuroBlate System first-in-humans Phase I clinical trial for recurrent glioblastoma