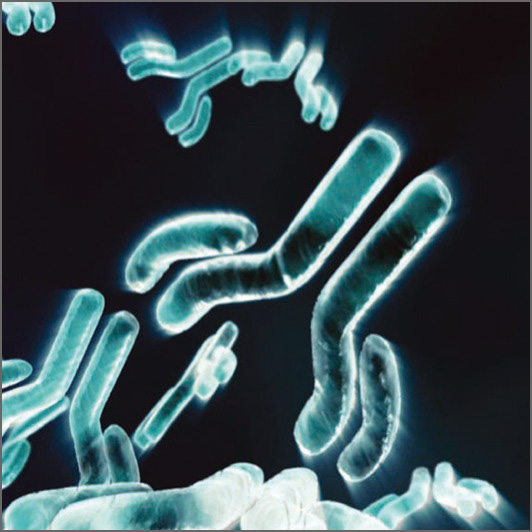
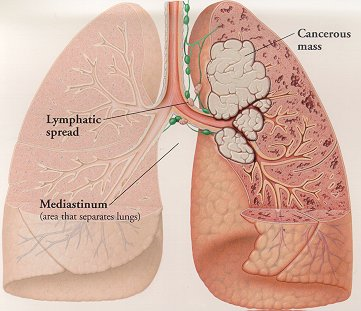
Systemic lupus erythematosus (SLE) is a complex autoimmune disease that afflicts tens of millions of people worldwide. The most prominent feature is generation of “autoantibodies” to self-proteins and nucleic acids, resulting in immune complex (IC) formation and organ inflammation. Affected patients may demonstrate rashes, joint pain, anemia, or kidney damage, and untreated complications can often be fatal. In addition, most SLE patients demonstrate continuously elevated levels of interferon (IFN) α, which is naturally produced by activated plasmacytoid dendritic cells (pDCs) 1. pDCs are a rare subset of DCs found in the blood and peripheral lymphoid organs that function in host defense by secreting proinflammatory cytokines to initiate the innate immune response. pDCs are activated following engagement of Toll-like receptors (TLRs), which recognize molecular signatures of bacteria and viruses. Studies have shown that the frequency of circulating pDCs is significantly reduced in SLE patients, due to increased migration to inflammatory sites in affected organs 2. Although pDCs have been implicated in contributing to autoimmunity via continuous type I IFN production, their exact role in lupus pathogenesis has not been clearly elucidated.
Systemic lupus erythematosus (SLE) is a complex autoimmune disease that afflicts tens of millions of people worldwide. The most prominent feature is generation of “autoantibodies” to self-proteins and nucleic acids, resulting in immune complex (IC) formation and organ inflammation. Affected patients may demonstrate rashes, joint pain, anemia, or kidney damage, and untreated complications can often be fatal. In addition, most SLE patients demonstrate continuously elevated levels of interferon (IFN) α, which is naturally produced by activated plasmacytoid dendritic cells (pDCs) 1. pDCs are a rare subset of DCs found in the blood and peripheral lymphoid organs that function in host defense by secreting proinflammatory cytokines to initiate the innate immune response. pDCs are activated following engagement of Toll-like receptors (TLRs), which recognize molecular signatures of bacteria and viruses. Studies have shown that the frequency of circulating pDCs is significantly reduced in SLE patients, due to increased migration to inflammatory sites in affected organs 2. Although pDCs have been implicated in contributing to autoimmunity via continuous type I IFN production, their exact role in lupus pathogenesis has not been clearly elucidated.
Recently, in PNAS, Baccala et al. provided direct evidence that in the absence of pDCs, the disease manifestations of Lupus were significantly decreased 3. Since IRF8 is a hematopoietic cell-specific transcription factor known to be essential for pDC development 4, the authors knocked out IRF8 in NZB mice, a widely used mouse model for SLE. Appropriately, pDCs were absent in IRF8-deficientNZB mice, and type I IFNs were undetectable even after injection with CpG DNA, a standard method of inducing the interferon pathway. Interestingly, autoantibody production was almost completely abrogated and kidney disease was drastically improved compared to wild-type NZB mice. Taken together, their results suggest that without pDCs, SLE disease manifestations are significantly reduced.
Next, the authors sought to examine specifically how pDCs promote systemic autoimmunity. They used another mouse model with a mutation in Slc15a4, which is characterized by normal development of pDCs but an absence of type I IFN production by pDCs. It is still unclear how a mutation in Slc15a4 leads to a disruption in proinflammatory cytokine production in pDCs, but since Slc15a4 is a peptide/histidine transporter, others hypothesize that it transports free histidine from the endosome to the cytosol to enable cathepsin-mediated cleavage of endosomal TLRs required for subsequent signaling 5. Similar to the IRF8-deficient NZB mice, Slc15a4 mice had significantly reduced autoantibodies, decreased kidney disease, and extended survival. This finding rules out the possibility that pDCs contribute to disease through other functions outside of type I IFN production.
In summary, Baccala et al. provide direct evidence that pDCs contribute to the abnormal manifestations of SLE via hyperproduction of type I IFNs. Thus, IRF8 and Slc15a4 serve as new potential drug targets for treatment of SLE. Current therapies involve broad immunosuppressive drugs, which suppress multiple arms of the immune system, increasing a patient’s risk for various infections and cancer. Specific pharmacologic inhibition of IRF8 or Slc15a4 could prevent Lupus-specific flare-ups, as well as manifestations of other autoimmune diseases.
References
1 Gilliet, M., Cao, W. & Liu, Y. J. Plasmacytoid dendritic cells: sensing nucleic acids in viral infection and autoimmune diseases. Nat Rev Immunol 8, 594-606, doi:10.1038/nri2358 (2008).
2 Ronnblom, L. The type I interferon system in the etiopathogenesis of autoimmune diseases. Ups J Med Sci 116, 227-237, doi:10.3109/03009734.2011.624649 (2011).
3 Baccala, R. et al. Essential requirement for IRF8 and SLC15A4 implicates plasmacytoid dendritic cells in the pathogenesis of lupus. Proc Natl Acad Sci U S A 110, 2940-2945, doi:10.1073/pnas.1222798110 (2013).
4 Tsujimura, H., Tamura, T. & Ozato, K. Cutting edge: IFN consensus sequence binding protein/IFN regulatory factor 8 drives the development of type I IFN-producing plasmacytoid dendritic cells. J Immunol 170, 1131-1135 (2003).
5 Park, B. et al. Proteolytic cleavage in an endolysosomal compartment is required for activation of Toll-like receptor 9. Nat Immunol 9, 1407-1414, doi:10.1038/ni.1669 (2008).











 With the increasing prevalence of neurodegenerative disorders in the aging population, it has become more and more important to understand the molecular pathways that regulate and advance these disorders. Due to the high level of complexity of the mammalian brain, it is very difficult to devise improved targeted treatments. The biggest limitation in neurodegenerative disease research being the lack of viable biomarkers for the elder population. Neurodegenerative disorders such as Alzheimer’s, Parkinson’s and polyglutamine diseases, share many pathogenic abnormalities such as the accumulation of misfolded proteins due to mutations rendering them resistant to degradation or over-expression of the wild type form.
With the increasing prevalence of neurodegenerative disorders in the aging population, it has become more and more important to understand the molecular pathways that regulate and advance these disorders. Due to the high level of complexity of the mammalian brain, it is very difficult to devise improved targeted treatments. The biggest limitation in neurodegenerative disease research being the lack of viable biomarkers for the elder population. Neurodegenerative disorders such as Alzheimer’s, Parkinson’s and polyglutamine diseases, share many pathogenic abnormalities such as the accumulation of misfolded proteins due to mutations rendering them resistant to degradation or over-expression of the wild type form.