In 1937, the cancer stem cell hypothesis was proposed to explain the concept of tumor heterogeneity (Clevers, 2011). In the mid 1990s, alongside the boom of stem cell biology, the theory that subpopulations of leukemia with stem cell-like properties was reintroduced with seminal work from John Dick (Clevers, 2011). These subpopulations were named “cancer stem cells” (although many today prefer the term “tumor-initiating cells”) due to their tumorigenicity and apparent self-renewal, thus mimicking the adult stem cell properties of multipotency and self-renewal. Today, cancer stem cell populations have been identified for cancers of the brain, pancreas, ovary, colon, liver, as well as leukemia (Magee et al, 2012). However, while confirmation of tumor-initiating cells in all tumors cannot be proven (Magee et al, 2012), the study of cancer stem cells remains important due to its possible impact on current cancer therapy.
In many tumors, cancer cell subpopulations are believed by many to be resistant to chemotherapy and radiation therapy (Clevers, 2011) (Magee et al, 2012). The importance becomes clearer when one looks at the possible outcome of not taking into account targeting cancer stem cells when developing cancer therapy. Computer simulations have shown that use of therapy that only targets non-tumorigenic cancer cells would enrich for the tumorigenic tumor-initiating cells, exacerbating the malignancy of many cancers (Vermeulen et al, 2012). This would explain why many cancers are more malignant after treatment with current therapy. In addition, the current intricacy of dealing with heterogeneity of the tumor is an issue since many different cancerous cell types respond differently to current therapies (Vermeulen et al, 2012) thus making ideal therapy difficult.
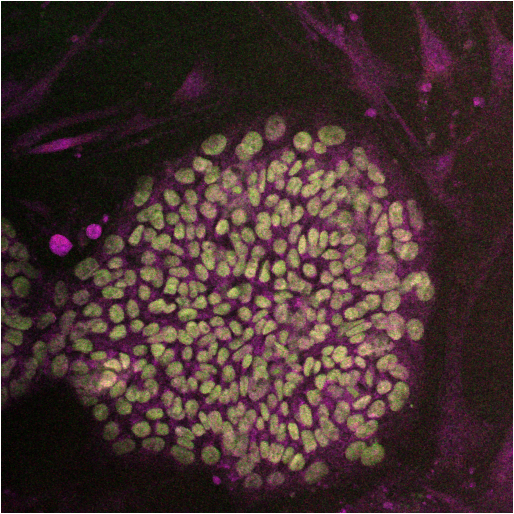
The cancer stem cell hypothesis is not the only theory to be brought forth to explain tumor heterogeneity. One belief is in the stochastic model of tumor heterogeneity, where variances in genetics and epigenetics cause the heterogeneity of tumor. Due to selection of more robust subpopulations, clonal evolution causes cell populations to proliferative non-uniformly in a tumor (Magee et al, 2012). Another proposed theory of tumor heterogeneity is the belief in the variation of extrinsic factors caused by the changes in the tumor microenvironment (Magee et al, 2012). In this model, cells that are closer to areas, such as the vasculature, form a niche that change the properties of tumor cells in a temporary, or permanent, manner (Magee et al, 2012). The cancer stem cell model states that a distinct subset of a tumor is tumorigenic and has the ability to self-renew (form more tumorigenic cells) or differentiate into the bulk of the non-tumorigenic cells of the tumor (Magee et al, 2012). Within the tumor-initiating cell community, there has been increasing support for a non-mutually exclusive model which has a combination of the hypotheses listed above that may contribute to tumor heterogeneity (Clevers, 2011)(Magee et al, 2012). One must account for all of these factors as possibilities when studying populations that may be tumorigenic inside a tumor model. For instance, attempting to study a certain population of ovarian cancer stem cells in vitro does not recapitulate the microenvironment and may negatively affect observation outcomes.
There have been many proposed mechanisms for identifying and studying cancer stem cells. These include the isolation of specific surface marker phenotypes, the use of cultures that are thought to favor the clonogenicity of the cancer stem cell population (such as the sphere forming cultures), serial transplantations of certain populations into immunocompromised mice to check tumorigenicity, and microscopic analysis of tumor heterogeneity through markers. However, there are limitations and caveats that one must consider when using these techniques to study cancer stem cell biology. First, studies have indicated that the cancer stem cell phenotype may be a context-specific event, showing up only in certain patient samples at certain ages (Magee et al, 2012). Furthermore, it is still unknown whether non-tumorigenic cells may become (through spontaneous formation or de-differentiation) tumorigenic cancer stem cells. This phenotypic plasticity calls into question the isolation of certain populations and the validity of ex-post facto tumor heterogeneity since confirmatory data to the initial isolation of a cancer stem cell population and subsequent studies would be lacking.
Therefore, if one were to study cancer stem cells, the key is to not rely too heavily on one assay, but to interweave all of the assays for bona fide tumor-initiating cell experimentation. For instance, one should study different populations of brain tumors, keeping in mind the limitations of their results, and be able to recapitulate their findings in a properly formed sphere formation assay as well as in an in vivo limited dilution model of tumorgenecity. Even to this end, the expression of cancer stem cells, both in number and property, may be extremely patient specific and rigorous testing of individual cases must be performed before any basic-science concepts are used for treatment.
Things to keep in mind when studying cancer stem cells:
- Although controversial, Cell surface markers have been correlated with a cancer stem cell phenotype, these include:
- Glioma: CD133, SSEA1, CD49f, Musashi-1, and Nestin
- Breast: BMI-1, CD44, CD24, CD49f, ALDHA1, and EpCAM
- Lung: ALDHA1, CD90, CD117, and EpCAM
- Upregulation of certain stem cell associated genes, such as Nestin, Oct4, Sox2, Nanog, Mushashi1, Notch1, and Notch4 have also been traditionally used to identify cancer stem cell subpopulations
- Multiple primary tumors tend to be better specimens to study compared to immortalized cancer cell lines, which have undergone many mutations through passages that may affect the representative phenotype of tumor-initiating cells.
- Many labs studying cancer stem cells agree that lineage tracing and side-by-side fate mapping of tumor subpopulations is essential for proper tumor-initiating cell studies.
- Single-cell, serial transplantation into immunocompromised mice, if feasible in your system, is an adequate assay to test for cancer stem cell phenotype. However, there are still possible issues of minor immunoediting in immunocompromised mice. If one is dealing with murine specimens, the use of a syngeneic mouse line may limit this issue.
- The possibility of quiescent cancer stem cells must be taken into account
- This can be studied looking at the cell population of interest and performing a western blot analysis on stem cell associated proteins (such as Sox2, Nestin, Oct 4, Nanog, etc.) with cell proliferation markers (increase of cell cycle regulators, such as p21, Cyclin D2, TP53 and a downregulation of cell cyclin proliferative markers such as Cyclin B1, cdc20, and Myc)(Moore and Lyle, 2011).
- Use label-retention/chase experiments, such as tritiated thymidine (3H-TdR) or 5-bromo-2-deoxy-uridine (BrdU), on your cell of interest is also a good technique and an in vivo alternative a (Moore and Lyle, 2011).
- Genetically engineered mouse models that spontaneously form tumors are tools that allow for the study of tumor-initiating cells while controlling for most artificial biases seen in engraftment of xenospecies cells and/or high-passage cancer cells. There is some concern whether artificial plastic culture conditions may affect the in vitro study of cell populations due to the lack of mechanical sensitivity found in the actual tumor microenvironment. This may be controlled for by assaying clonal analysis on a 3D scaffold system that is representative of the primary location of the tumor (Pastrana et al, 2011).
- Sphere formation assays may select against tumor initiating cells that do not form spheres (Read and Wechsler-Reya, 2012).
Suggested Reading/ References:
The cancer stem cell: premises, promises, and challenges. Clevers H. Nature Medicine 2011 Mar 7:17(3).
Cancer Stem Cells: Impact, Heterogeneity, and Uncertainty. Magee JA, Piskounova E, Morrison SJ. Cancer Cell 2012 Mar 20:(21).
The developing cancer stem-cell model: clinical challenges and opportunities. Vermeulen L, De Sousa e Melo F, Richel DJ, Medema JP. Lancet Oncology Feb: (13):e83-89.
Quiescent, Slow –Cycling Stem Cell Populations in Cancer: A Review of Evidence and Discussion of Significance. Moore N and Lyle S. Journal of Oncology, 2011.
Spheres without Influence: Dissociationg In Vitro Self-Renewal from Tumorigenic Potential in Glioma. Read TA, Wechsler-Reya RJ. Cancer Cell, 2012 Jan 17: (21).
Eyes Wide Open: A Critical Review of Sphere-Formation as an Assay for Stem Cells. Pastrana E, Silva-Vargas V, Doetsch F. Cell Stem Cell May6:(8).