Alzheimer’s disease (AD) is the most common form of dementia typically presenting itself after the age of 60, due to protein misfolding in the brain. According to the National Institute on Aging, currently it is estimated that 5.1 million Americans suffer from AD. Dimentia, is defined as the loss of cognitive function including thinking, remembering, reasoning abilities, and behavioral abilities. The severity of the disease ranges from pre-dementia (early onset) characterized by small affects on a persons functioning all the way to advanced where a person requires complete dependence on others for daily living.
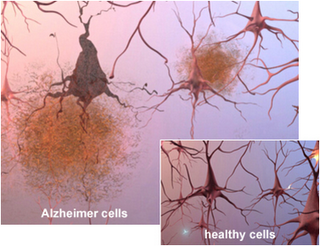
AD was originally identified by Dr. Alois Alzheimer in 1906 after a brain biopsy of a woman showed abnormal clumps in her brain, now known as Amyloid plaques. Amyloid plaques originate from amyloid-β (Aβ) deposits which are insoluble fibrous protein aggregates arising from misfolded proteins and polypeptides.
The dominant hypothesis for AD neuropathology is that Aβ plaque formations initiate a cascade that is followed by loss of neurons and synapses in the cerebral cortex and central subcortical regions as well as abnormal levels of neurotransmitters acetylcholine (decreased levels, leading to decreased cognition) and glutamate (increased levels, leading to neuronal over-activation and cell death). The combined effects being progressive cell death in select regions of the brain. Currently available treatments for AD include drugs that target acetylcholine, glutamate and the amyloid cascade pathway. These treatments are only efficacious at treating some of the symptoms they don’t stop the underlying decline and death of neurons. Additionally, it is now believed that Aβ plaques are necessary but not sufficient for the cognitive and neurodegenerative effects seen in AD patients. Therefore, the lack of efficacy in currently available treatments and the much needed understanding of the secondary effects due Aβ plaques, shows there is a dire need for safer and more efficacious therapies which can delay and reverse the effects of AD as well as modulate neuronal function in the affected neural circuits.
In a recent TEDx Talk, Dr. Andres M. Lozano from the Toronto Western Research Institute (TWRI) talks about a novel technology used for treating neuronal disorders, deep brain tissue stimulation (DBS). Dr. Lozano’s team have studied the effects of DBS on a variety of neurodegenerative disorders including AD and Parkinson’s disease showing exciting breakthroughs. DBS is surgical procedure where a brain pacemaker is implanted in an affected region of the brain. The pacemaker can then be controlled externally and directed to send electrical impulses to a specific location.
The human brain consumes about 25% of the total body glucose levels. In AD patients, it is well known that glucose uptake/metabolism is significantly impaired. Using positron emission tomography (PET) scans with the radiotracer [18F]-2-deoxy-2-fluoro-D-glucose (measures regional cerebral glucose metabolism) Dr. Lozano’s team found that DBS resulted in increased glucose metabolism in AD patients after 1 yr of treatment (http://clinicaltrials.gov/show/NCT00658125). More importantly, the increased metabolism correlated with better outcomes in global cognition, memory, and quality of life. Based on preclinical studies, it is believed that DBS functions by inducing the generation of new neurons through electrical impulses. Although, the effects of DBS on Aβ breakdown remain unclear and are under investigation in preclinical models.
It is important to note that not all patients displayed the same level of benefit from DBS. In addition, all patients in this study had relatively mild AD and higher basal levels of cognitive function and glucose compared to more advanced patients. Therefore, it is possible that the effects of BDS in advanced AD patients will not be as beneficial, although this remains to be determined. It will be interesting to see what the long term effects of DBS will be and whether BDS will be sufficient to keep AD progression at bay.
Further Reading:
Increased Cerebral Metabolism After 1 Year of Deep Brain Stimulation in Alzheimer Disease. Gwenn S. Smith, Adrian W. Laxton, David F. Tang-Wai, Mary Pat McAndrews, Andreea Oliviana Diaconescu, Clifford I. Workman, Andres M. Lozano. Arch Neurol. 2012;69(9):1141-1148. doi:10.1001/archneurol.2012.590.
Memory rescue and enhanced neurogenesis following electrical stimulation of the anterior thalamus in rats treated with corticosterone. Clement Hamani, Scellig S. Stone, Ariel Garten, Andres M. Lozano, Gordon Winocur. Experimental Neurology.Nov;232(1):100-104. doi: 10.1016/j.expneurol.2011.08.023.