Cell replacement therapy (CRT) and cell-based therapy (CBT) have provided promising therapeutic strategies for treatment of several human neurological diseases such as Parkinson’s disease (PD), Huntington’s disease (HD), multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), Alzheimer’s disease (AD) and malignant gliomas (GBM). The four most-studied cell types considered viable candidates for development of CRT and CBT for these neurological diseases consist of embryonic stem cells (ESCs), induced pluripotent stem cells (iPSCs), mesenchymal stem cells (MSCs) and neural stem cells (NSCs). Although generation of different types of neurons and glial cells in vitro have been demonstrated by all these pluripotent cells, there are significant obstacles to the clinical utilization of stem cell-derived neurons or glial cells in CBT: First concern, aroused by previous studies, involves the long- term survival and phenotypic stability of stem cell-derived neurons or glial cells in vivo following transplantation. Second limitation is the high risk of any highly purified populations of neuronal cell type derived from ESCs, iPSCs, MSCs or NSCs, containing other neuronal/glial cell types, which may cause unfavorable interactions among grafted cells and/or with host central nervous system (CNS). Finally, the subpopulation (regardless of how small) of ESCs, iPSCs, MSCs or NSCs that did not completely differentiate, introduce a significant risk of tumorigenesis within the host CNS following transplantation. Furthermore, there are practical caveats, such as sustainable clinically approved, industrial quantity of these cells, which remain to be addressed.
In a recent review article published in the Journal of Neuropathology Seung U. Kim’s group have proposed utilization of immortalized human NSC lines as the cell-source for CBT in neurological diseases, as the best suited candidate. Kim’s group have previously generated clonally derived several immortalized human NSC lines, one of which has been particularly well characterized and currently used as a glioma therapy agent in phase II clinical trials. This particular line, named HB1.F3, was originally obtained from a fetal human telencephalon at 15 weeks gestation and immortalized by an amphotropic replication-incompetent retroviral vector, pLCN.v-myc, which encodes the v-myc oncogene. This method of immortalization is not only safe, but also overcomes the issue of spontaneous differentiation, resulting in a non- tumorigenic, homogeneous NSC line.

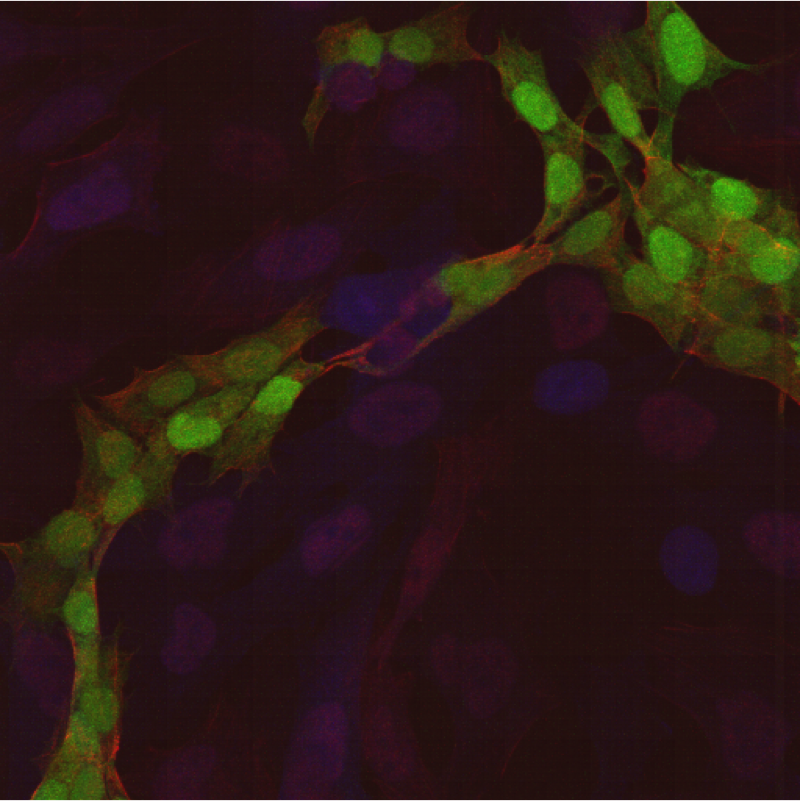
HB1.F3’s exhibit normal human karyotype of 46XX, they are self-renewing and multipotent, capable of differentiating into neurons, astrocytes and oligodendrocytes, both in vivo and in vitro. They express genes that encode for neurotrophic factors, such as for nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), neurotrophin-3 (NT-3), glial-derived neurotrophic factor (GDNF), ciliary neurotrophic factor (CNTF), hepatocyte growth factor (HGF), insulin-like growth factor (IGF)-1, basic fibroblast growth factor (bFGF), and vascular endothelial growth factor (VEGF), which can potentially make them a therapeutic agent rendering neuroprotection for neurons affected by injury or disease.
Kim’s group has reported functional improvement in a rat model of PD following HB1.F3 transplantation into the striatum. In yet another study, they show functional recovery in HD rat model, upon intravascular (iv) administration of HB1.F3s; their data suggests that the improvements observed here is due to the neuroprotection provided by HB1.F3s’ secretion of BDNF, since this factor has been previously shown to block neuronal injury under pathological conditions in animal models of HD. Another interesting outcome to this study is the integration of HB1.F3s in the striatum and homing to the site of neuronal injury, following their iv administration, indicative of their ability to freely cross the BBB.
In AD patients, low levels of acetylcholine (ACh) is one contributing cause of cognitive impairment. The lack of sufficient ACh is due to the decreased activity of choline acetyltransferase (ChAT) that synthesizes ACh. Kim’s group transduced HB1.F3s, over-expressing the ChAT gene (F3.ChAT) and transplanted these NSCs into the brain of AD animal models. Their results show the functional recovery of presynaptic cholinergic system and fully restored learning and memory. Moreover, they generated motor neurons from HB1.F3s- encoding Olig2 basic helix loop helix (bHLH) transcription factor gene with sonic hedgehog (Shh) protein (F3.Olig2-Shh)- and transplanted them into L5 of the spinal cord of ALS animal model. This resulted in significantly delayed onset of the disease and prolonged average survival.

Utilization of HB1.F3s in human clinical trials was one of the first FDA permitted clinical trials in the United States, to use genetically modified human stem cells in maligant brain tumor CBT. Furthermore, the findings reported here do indicate that immortalized human NSCs are an effective source of cells for genetic manipulation and gene transfer into the CNS, for treatment of several neurological disorders. However, autologous iPSC-derived CNS cells seem to be a more promising strategy for CRT. This is mainly due to the risks associated with introducing immortalized cells, which may not survive long term post-transplantation. Nonetheless, all the mentioned stem cell sources have interesting characteristics that make each type suitable for treating different disorders.
Further Reading:
Neural Stem Cell-Based Treatment for Neurodegenerative Diseases