Human peripheral blood mononuclear cells (PBMC) are comprised of complex populations of T cells, B cells, NK cells, monocytes, and dendritic cells. In addition, there are more complicated cell types such as NKT cells that are thought of as T cells that share many properties of NK cells. Within all of these basic populations are many functionally unique subsets. Because of the diversity of populations in PBMC, flow cytometry represents the best method for studying functional and phenotypic properties of these cell subsets. In the next few blog posts, I will discuss selection of markers for studying PBMC populations using flow cytometry and the best way to arrange these markers in flow cytometry staining panels.
The PBMC cell type I have the most experience with characterizing is T cells. CD3, a T cell specific marker, is necessary to differentiate T cells from other populations, simply because CD4 and CD8 can be expressed by other cell types. CD8 can be expressed on NK cells, while CD4 can be expressed on populations of monocytes and dendritic cells. CD4 and CD8 are also necessary markers for identification of these two major T cell populations.
CD4 and CD8 T cells are most simply classified as naïve or antigen experienced populations including central memory, effector memory and effectors. Central memory and effector memory populations are known to differ in their effector functions and ability to home to different anatomical sites. Two markers are necessary to differentiate naive, central memory, effector memory and effector T cell populations present in PBMC.
The first is CD45, a protein tyrosine phosphatase regulating src-family kinases, is expressed on all hematopoietic cells. CD45 can be expressed as one of several isoforms by alternative splicing of exons that comprise the extracellular domain. CD45RA is expressed on naïve T cells, as well as the effector cells in both CD4 and CD8. After antigen experience, central and effector memory T cells gain expression of CD45RO and lose expression of CD45RA. Thus either CD45RA or CD45RO is used to generally differentiate the naïve from memory populations.
However, differentiation between central and effector memory populations and between naïve and effector populations can be achieved by adding a second marker. There are several markers that have been used for this purpose and these tend to mark these populations at slightly different stages of the differentiation pathway that is thought to occur in T cells as they change from central to effector memory cells. The chemokine receptor CCR7 is considered the gold standard for this discrimination, and the lymph node homing receptor CD62L is a close second choice. Naïve and central memory cells express these receptors in order to migrate to secondary lymphoid organs, while the absence of these receptors allows for effector memory and effector cells to accumulate in peripheral tissues. CCR7 has been classically thought to be difficult to stain for due to low expression levels, and as a result I have never used it. However, a recent review article pointed out that a new brighter staining antibody to CCR7 has been developed (clone 150503), and is something I hope to test in the near future. CD62L has generally been my marker of choice, however CD62L expression is lost following density gradient centrifugation, cryopreservation, TCR ligation or activation with PMA/ionomycin. Thus CD62L as a marker is best utilized following overnight culturing subsequent to thawing cryopreserved cells. Other potential markers are CD27 and CD28 which are also more highly expressed by the central memory and naive populations. However, it is important to note that each of these markers, CCR7, CD62L, CD27, and CD28, marks slightly different populations of cells and care must be taken when making comparisons between populations defined by different markers for assessing frequencies or functions.
In summary, naïve T cells are CD45RA+CD45RO–CCR7+CD62L+, central memory T cells are CD45RA–CD45RO+CCR7+CD62L+, effector memory T cells are CD45RA–CD45RO+CCR7–CD62L–, and effector cells are CD45RA+CD45RO–CCR7–CD62L–. Thus, CD3, CD4, CD8, CD45RA or CD45RO, and CCR7 or CD62L or CD27, are a great starting point for designing flow cytometry panels for the assessment of T cells present in human PBMC. T cells populations, however, are much more complex, and may be further classified by helper subtypes and activation status, which will be discussed in a later blog.

The use of CD45RA and CD62L to differentiate naive, central memory, effector memory and effector T cell populations present in PBMC. Naïve CD4 and CD8 T cells are CD45RA+CD45RO–CCR7+CD62L+ (B, F), central memory T cells are CD45RA- CD45RA–CD45RO+CCR7+CD62L+ (A, E), effector memory T cells are CD45RA–CD45RO+CCR7–CD62L– (C, G), and effector cells are CD45RA+CD45RO–CCR7–CD62L– (D, H).
Further Reading:
Central memory and effector memory T cell subsets: function, generation, and maintenance. Sallusto F, Geginat J, Lanzavecchia A. Annu Rev Immunol. 2004;22:745-63.

 Even though, iPSCs can be generated reproducibly, the efficiency of the reprograming remains low (i.e., around 1% using the original method). Furthermore, the initial generation of iPSCs utilized either retroviruses or lentiviruses, which both integrate into the host genome and might cause insertional mutagenesis, collectively creating a risk for translational applications. However, the beauty of the iPSC technology is its simplicity and reproducibility. Since 2007, iPSCs have been in the central focus of stem cell research and regenerative medicine, and researchers throughout the world have made a number of improvements to Yamanaka’s original protocol. Today, we have safer and more efficient methods for generation human iPSCs for disease modeling or cell replacement therapies, and by the look of how much has been achieved so far, the technology is only going to get better and more proficient. Considering that human embryonic stem cell derived approaches have been successfully used at the clinical level for cell replacement therapies, there is no doubt that iPSCs will eventually prove to be the ultimate source for regenerative medicine in the future.
Even though, iPSCs can be generated reproducibly, the efficiency of the reprograming remains low (i.e., around 1% using the original method). Furthermore, the initial generation of iPSCs utilized either retroviruses or lentiviruses, which both integrate into the host genome and might cause insertional mutagenesis, collectively creating a risk for translational applications. However, the beauty of the iPSC technology is its simplicity and reproducibility. Since 2007, iPSCs have been in the central focus of stem cell research and regenerative medicine, and researchers throughout the world have made a number of improvements to Yamanaka’s original protocol. Today, we have safer and more efficient methods for generation human iPSCs for disease modeling or cell replacement therapies, and by the look of how much has been achieved so far, the technology is only going to get better and more proficient. Considering that human embryonic stem cell derived approaches have been successfully used at the clinical level for cell replacement therapies, there is no doubt that iPSCs will eventually prove to be the ultimate source for regenerative medicine in the future.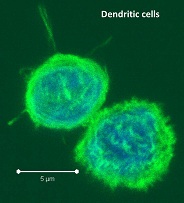

 The immune system is the body’s primary defender against cancer. In a recent article in Science magazine,
The immune system is the body’s primary defender against cancer. In a recent article in Science magazine,