Cytology is a key component in diagnosis and screening of diseases such as cancer. It assesses single cells and clusters of cells from sources such as malignant effusions and peripheral blood. Effusions are fluids that leak from blood and lymph vessels and aggregate in tissues and cavities within the body. This is a common problem in cancer patients and can be a reservoir of malignant cells. However, the total number of cells in effusions is small in comparison to the volumes of fluids that are produced. Therefore, in order to collect these cells for evaluation, they must be concentrated.
Cytospin is a cytology method that is specifically designed to concentrate cells such as these that are found in small numbers. After the cytospin is completed, other cytology methods such as immunocytochemistry can be preformed to evaluate the cells. An example is a recent study from Ikeda et al., in which immunocytochemical staining of cytospins from malignant effusions suggested that EMA, IMP3, and GLUT-1 might be helpful in distinguishing malignant cells from benign cells (1). The cytospin process is a simple procedure. Cells are washed in a serum and/or albumin based PBS or culture media solution. The cells are resuspended in up to 500 µl of this solution. A cytofunnel is attached to a glass slide and slide carrier. The entire apparatus is inserted into a cytocentrifuge and the cell suspension is added.
The cells can be spun at various speeds and times depending on the cell type. Eight hundred rpm for up to 5 minutes is a good place to start. The volume to cell ratio must be dilute enough to ensure formation of a monolayer of cells for the best assessment of the cells.
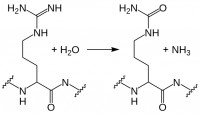
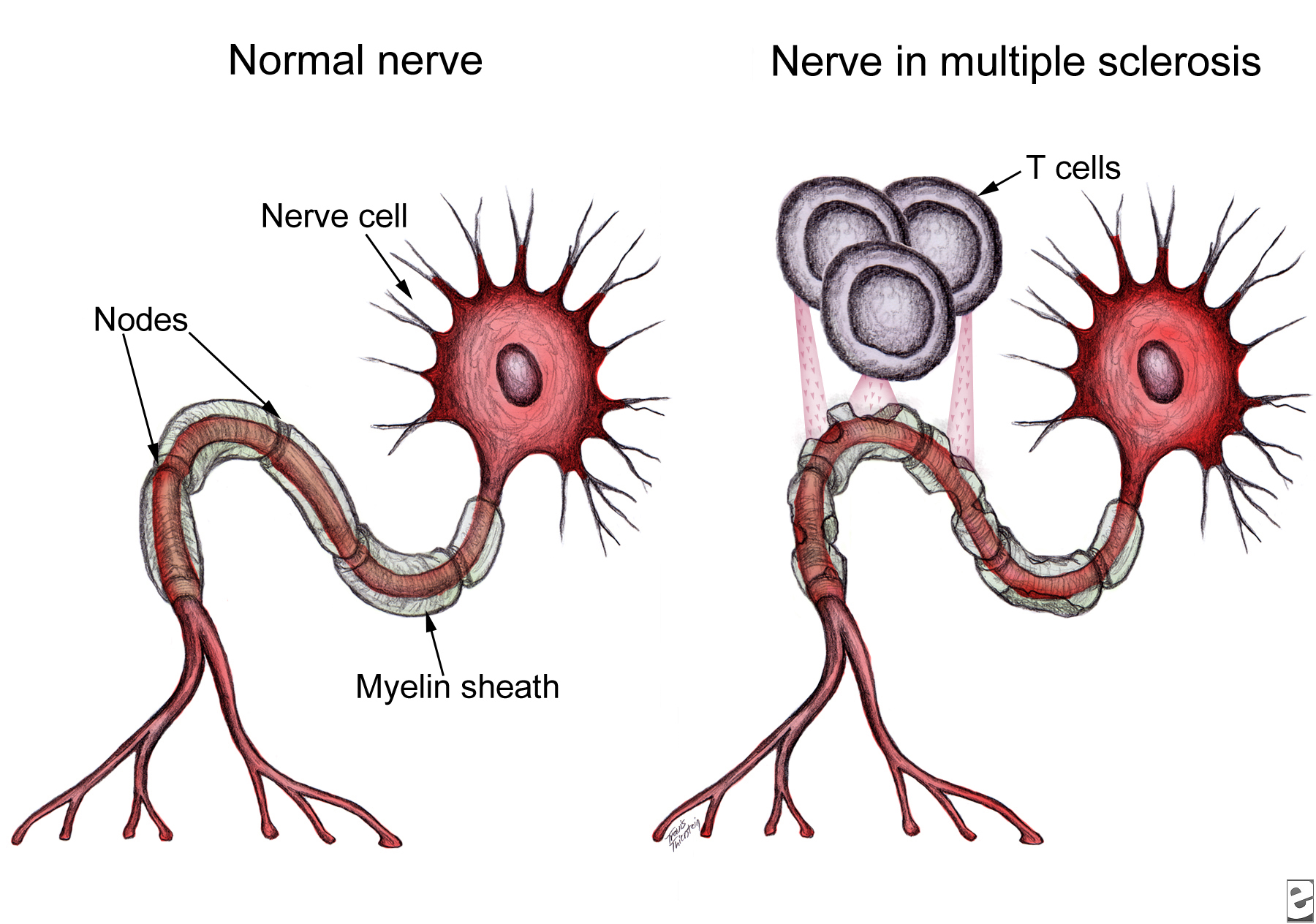
In the Ikeda et al. study, cytology was used to differentiate benign mesothelial cells from malignant mesothelial cells (1). What are mesothelial cells and why is it important to distinguish between benign and malignant forms? These are cells that make up the epithelial lining of the mesothelium which covers the surface of the peritoneal, pericardial, pleural cavities as well as the organs within the cavities (2). The mesothelium has many functions. It is a protective barrier against physical damage and invading organisms as well as being a frictionless interface for free movement of organs and tissue (2). Other functions include roles in fibrinolysis and coagulation, initiation and resolution of inflammation and tissue repair, antigen presentation, transport of fluid and cells, and tumor cell adhesion and growth (2). Reactive mesothelial cells (benign cells) appear in instances when there is a pathogenic infection or physical trauma. Malignant mesothelioma is a rare cancer of mesothelial cells. In effusions, it is sometimes difficult to distinguish benign cells from malignant cells especially when there are few cell numbers. However, immunocytochemistry performed on cytospin cells helps to differentiate these cells. Biomarkers such as epithelial membrane antigen (EMA), glucose transporter-1 (GLUT-1), and insulin-like growth factor-II mRNA-binding protein 3 (IMP3) are useful in separating benign cells from malignant cells. EMA is a large cell surface glycoprotein, also known as MUC1, expressed by glandular and ductal epithelial cells as well as some hematopoietic cells. It has a protective and regulatory role by acting as a barrier to the apical surface of epithelial cells. GLUT-1 is a protein that assists in the transport of glucose across the plasma membrane of cells. It is decreased when glucose levels are high and increased when levels are low. IMP3 binds to sequences in the 3’-UTR of CD44 mRNA. CD44 has a role in cell migration, cell adhesion, and cell-cell interactions. In the Ikeda study, EMA staining intensity on cytospins of malignant mesothelioma cells was strong but staining in reactive cells was weak. EMA stained both the cytoplasm and the membrane of the cells. GLUT-1 stained the membrane of the cytospin cells and expression was highly sensitive in malignant cells. IMP3 stained the cytoplasm of the cytospin cells and expression was lowest in malignant cells. Although these markers help to differentiate malignant from reactive cells, they should not be used as standalone markers. This is because there is no individual biomarker that is exclusively sensitive and specific enough to discriminate between these cells.
Overall, the cytospin technique is a quick method to collect and concentrate fluids that contain a low number of cells. When performing immunocytochemistry after cytospins one can use the same staining protocol used to stain samples from tissue blocks. Cytospins can also be used to take a closer look at cellular staining from cells that have been processed for flow cytometry. This is an excellent method to provide a first look at the immunopathology of a cell. For subsequent postings, the cytospin process will be dissected by discussing key steps and methods of troubleshooting.
Further Reading:
1. Ikeda, K., Tate, G., Suzuki, T., Kitamura, T. & Mitsuya, T. Diagnostic usefulness of EMA, IMP3, and GLUT-1 for the immunocytochemical distinction of malignant cells from reactive mesothelial cells in effusion cytology using cytospin preparations. Diagn Cytopathol 39, 395-401, doi:10.1002/dc.21398 (2011).
2. Mutsaers, S. E. The mesothelial cell. Int J Biochem Cell Biol 36, 9-16 (2004).









 recent edition of Nature Cell Biology Calvo et al. demonstrated that 6. Not only do the authors demonstrate that YAP/TAZ is active in CAFs, but YAP/TAZ is necessary for CAF development6. They show that CAF activation leads to matrix remodeling towards increased stiffness, via myosin light chain 2 (
recent edition of Nature Cell Biology Calvo et al. demonstrated that 6. Not only do the authors demonstrate that YAP/TAZ is active in CAFs, but YAP/TAZ is necessary for CAF development6. They show that CAF activation leads to matrix remodeling towards increased stiffness, via myosin light chain 2 (


