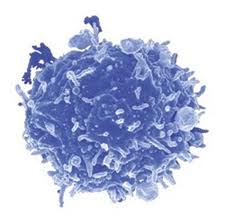
Recently a number of studies have arisen characterizing  various functional subsets of CD4+ FoxP3+ regulatory T cells (TREGS), as well as their plasticity and ability to differentiate into other TH subtypes. For instance, TREGS that express RORγt were found to be the specific TREG subset that promotes pro-tumor immune functions in colorectal cancer patients. In a recent article in Immunity, Sharma et al. identify another TREG subset: FoxP3+ TREGS that loose expression of Eos convert to a pro-inflammatory helper subtype that promotes naïve CD8+ T cells differentiation into potent effectors.
various functional subsets of CD4+ FoxP3+ regulatory T cells (TREGS), as well as their plasticity and ability to differentiate into other TH subtypes. For instance, TREGS that express RORγt were found to be the specific TREG subset that promotes pro-tumor immune functions in colorectal cancer patients. In a recent article in Immunity, Sharma et al. identify another TREG subset: FoxP3+ TREGS that loose expression of Eos convert to a pro-inflammatory helper subtype that promotes naïve CD8+ T cells differentiation into potent effectors.
Eos is a transcription factor in the Ikaros family, and acts as an obligate co-repressor in complex with FoxP3 to inhibit expression of FoxP3-repressed genes. In a quest to understand why TREGS in inflammatory environments were observed to become pro-inflammatory without losing FoxP3 expression, Sharma et al. examined the expression of Eos in FoxP3+ TREGS under inflammatory conditions.
Conversion of FoxP3+ TREGS into an inflammatory phenotype was demonstrated by acquired expression of IL-2, IL-17, and CD40L in the draining lymph nodes of a vaccination site compared with FoxP3+ TREGS at distant lymph nodes that did not gain this function. In these converted inflammatory FoxP3+ TREGS, expression of Eos was rapidly lost. IL-6 was required for downregulation of Eos, as TREGS in mice lacking IL-6 did not lose Eos expression under the same conditions. However, IL-6 alone was insufficient for Eos downregulation, which also required interactions with MHC class II on activated dendritic cells. Loss of Eos expression was furthermore shown to be required for acquisition of the pro-inflammatory phenotype, as TREGS with forced overexpression of Eos did not undergo this conversion.
Interestingly, not all FoxP3+ TREGS were equivalent in their propensity to lose Eos expression and become pro-inflammatory. Thymic FoxP3+ TREGS were assessed for stability of Eos under treatment with cyclohexamide. CD38+CD69+CD103– TREGS were “Eos-labile” and specifically lost Eos expression within one hour of cyclohexamide treatment, while CD38–CD69–CD103+ TREGS maintained Eos expression. Expression of other markers associated with FoxP3+ TREGS including CD25 and CTLA-4 were equivalent between these two phenotypes highlighting the inability of using these TREG markers to discriminate between these populations. When these FoxP3+ TREGS were sorted into CD38+CD103– and CD38–CD103+ subsets and transferred into mice, followed by the vaccination schema, only CD38+CD103– TREGS lost Eos expression and gained CD40L and IL-2 expression. The Eos-labile TREGS do however have characteristic suppressive functions when examined in several models including protection from colitis in a Rag-deficient CD45RBHI effector cell-driven autoimmune colitis model and in vitro suppression of T cell proliferation driven by anti-CD3.
Because the Eos-labile subset was observed in the thymus as part of the natural TREG repertoire, the authors examined the signals required for development of this subset. Again, IL-6 was required as this subset did not arise in IL-6-/- mice. Epigenetic analysis of DNA methylation patterns comparing these FoxP3+ TREGS subsets revealed distinctive patterns of methylation yet these subsets were still much more closely related to each other as compared with FoxP3– CD4+ T cells. Future studies will be needed to determine the nature of these epigenetic differences and which signals are controlled by IL-6.
Interestingly, the authors explored the functional contribution of the Eos-labile pro-inflammatory TREGS subset on CD8+ priming in the vaccination model. Depletion of TREGS resulted in loss of CD8+ T cell proliferation and granzyme B expression as well as loss of CD86 upregulation on DCs, while adding back just the Eos-labile subset or IL-2 plus CD40-agonist antibodies rescued these defects. The Eos-labile subset did not however, contribute to reactivation of memory CD4+ T cells, and thus these cells appear to play a specific role in the initial priming stages of naïve T cell activation. Thus, despite having regulatory activity, these cells are critical in priming CD8+ T cell responses by supplying IL-2 and CD40L signals.
However, indoleamine 2,3-dioxygenase (IDO) was able to block Eos downregulation and acquisition of IL-2, IL-17, and CD40L expression. Importantly, in a murine tumor vaccination model, blocking IDO was important for FoxP3+ inflammatory TREG induction and acquisition of anti-tumor effector CD8+ T cell responses. The mechanism of IDO inhibition of Eos downregulation was found to be at least in part, dependent on the antagonization of the IL-6-STAT3 pathway by IDO-mediated production of kynurenine-pathway metabolites which activate the aryl hydrocarbon receptor (AhR). Interestingly, different AhR ligands have been previously shown to differentially regulate induction of TH17 cells vs. TREGS (Quintana et al.), and kyenurine was a TREG inducing AhR ligand (Mezrich et al.). Additionally, the contrasting effects of IL-6 and IDO will be an important factor in priming immune cell responses.
Overall, this thorough investigation identified the mechanisms that induce and inhibit this newly defined Eos-labile TREG subset that maintains FoxP3 expression and has typical suppressive TREG activity, yet is critically important in priming effector T cell immune responses. Future studies will be needed to address how these cells balance regulatory and priming activities as well as the relationships between this subset and the many other TREG subsets described.
An inherently bifunctional subset of foxp3(+) T helper cells is controlled by the transcription factor eos. Sharma MD, Huang L, Choi JH, Lee EJ, Wilson JM, Lemos H, Pan F, Blazar BR, Pardoll DM, Mellor AL, Shi H, Munn DH. Immunity. 2013 May 23;38(5):998-1012. doi: 10.1016/j.immuni.2013.01.013. Epub 2013 May 16.
Eos, goddess of treg cell reprogramming. Rieder SA, Shevach EM. Immunity. 2013 May 23;38(5):849-50. doi: 10.1016/j.immuni.2013.05.001.
Control of T(reg) and T(H)17 cell differentiation by the aryl hydrocarbon receptor. Quintana FJ, Basso AS, Iglesias AH, Korn T, Farez MF, Bettelli E, Caccamo M, Oukka M, Weiner HL. Nature. 2008 May 1;453(7191):65-71. doi: 10.1038/nature06880. Epub 2008 Mar 23.
An interaction between kynurenine and the aryl hydrocarbon receptor can generate regulatory T cells. Mezrich JD, Fechner JH, Zhang X, Johnson BP, Burlingham WJ, Bradfield CA. J Immunol. 2010 Sep 15;185(6):3190-8. doi: 10.4049/jimmunol.0903670. Epub 2010 Aug 18.