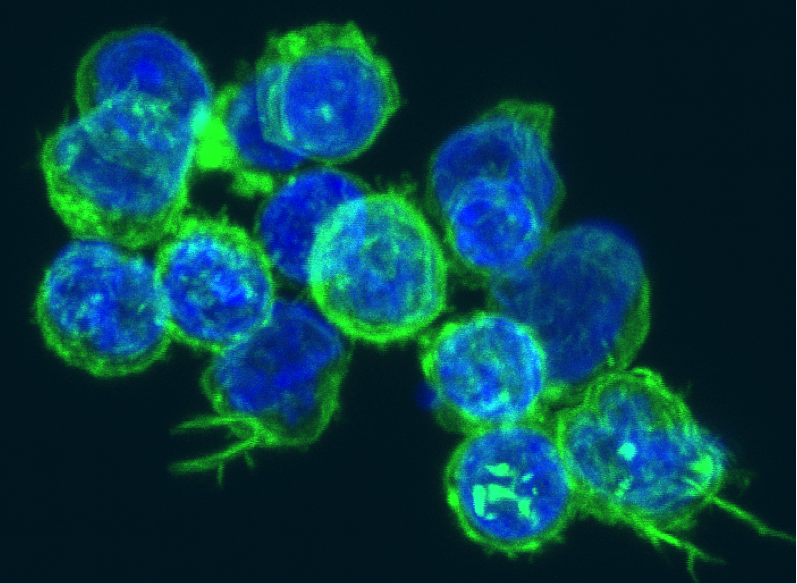
Multiple sclerosis (MS) is a chronically progressive, neuroinflammatory autoimmune disease of the central nervous system (CNS), mediated in part by CD4+ T-cells, which have escaped regulation and recognize myelin protein peptides.
CD4+ CD25+ regulatory T-cells (Tregs) are a subpopulation of suppressor T-cells that play a major role in maintenance of peripheral immune tolerance by active suppression of potential auto-aggressive T-cells. In contrast to patients with secondary progressive MS (SPMS) who have normal Treg function, patients with relapsing-remitting MS (RRMS) have functionally impaired Tregs; this lack of regulatory suppression leads to the infiltration of pathogenic CD4 T-cells into the CNS and the subsequent neuroinflammation.
Although patients with RRMS have a lower Treg number and function, previous studies have shown no correlation between therapeutic response and increased Treg number. However, based on data obtained from several autoimmune animal models, it has been speculated that the resistance of pathogenic CD4+ effector T cells (Teffs) to suppression by Tregs may be responsible for the failed tolerance in autoimmunity. Moreover, Teff resistance has been reported in some human autoimmune diseases such as type 1 diabetes mellitus (T1D), rheumatoid arthritis (RA), and psoriasis. Teff resistance is stimulated by several factors, including tumor necrosis factor–α (TNF-α), interleukin-4 (IL-4), IL-12, IL-6, IL-7, IL-15, IL-21 and the maturation state of CD4 T-cells.
In a recent study published in Nature, Schneider’s group demonstrated the presence of Teff resistance in individuals with aggressive RRMS and the role of interleukin-6 (IL-6) in promoting Teff resistance to Tregs.

Previous studies have shown the implication of IL-6 in MS pathology; IL-6 has been shown to inhibit apoptosis in T-cells, it is required for the differentiation of T-helper 17 (TH17) cells, and local exposure to IL-6 can result in the development of Teffs resistant to suppression. During establishment of an immune response-derived inflammation, IL-6 levels elevate rapidly and bind to the IL-6 receptor α (IL-6Rα) on the CD4 T-cell’s surface. Next Glycoprotein 130 (gp130) is recruited to this IL-6-IL-6R complex, which results in activation and phosphorylation of the signal transducer and activator of transcription 3 (STAT3). Otherwise, IL-6 cytokine can bind soluble IL-6Rα (sIL-6Rα) in the serum and induce the phosphorylation of STAT3 by forming a complex that signals through membrane-bound gp130. In addition to the genetic correlation between variants in the STAT3 locus and MS susceptibility, a significant increase in phosphorylated STAT3 (pSTAT3) as well as IL-6Rα expression on CD4+ T cells, have been reported in RRMS patients.
In Schneider’s recent study, the role of Teff resistance in RRMS’s failed tolerance was investigated by comparing Teffs from RRMS patients and healthy individuals, via Treg suppression assays; the obtained results show that Teff resistance is present only in the Teffs of RRMS patients with active disease (two or more clinical exacerbations or presence of one or more gadolinium-enhancing lesions on MRI within 2 years of sampling) and not those with inactive/mild disease.
Furthermore, by performing suppression assays in the presence of the STAT3 inhibitor (blocking STAT3 phosphorylation), they observed enhanced suppression, indicating a positive correlation between the degree of Teff resistance and increased pSTAT3 in response to IL-6; their data imply that an increase in IL-6Rα expression on CD4+ T-cells and enhanced IL-6–mediated phosphorylation of STAT3 are major contributors to the impaired suppression observed among their RRMS subjects. They hypothesized that in active RRMS patients, the increased pSTAT3 and resistance of the pathogenic CD4 T-cells to regulation mediated by Tregs, is due to the elevated IL-6 production by microglia, astrocytes, endothelial cells, neurons, oligodendrocytes, or infiltrating T-cells in the CNS.
Schneider’s new findings suggest utilization of IL-6Rα expression and IL-6 mediated pSTAT3 as new therapeutic markers for determining disease activity as well as evaluating responsiveness to immunomodulatory therapies, such as tocilizumab (an IL-6Ra antagonist) in RRMS. Another significant aspects of this study is the unconventional technical approaches utilized in assessing the impact of IL-6 on suppression within an antigen-presenting cells (APCs)-free system, as well as ensuring consistency of activation and source of Tregs via a bead-based stimulation assay and in vitro–generated Tregs respectively. These unique techniques are key to the conclusions drawn from this study and useful for future MS research.
Further Reading: