A study recently published in The New England Journal of Medicine (Jun 1st, 2013) identified an acquired mutation in the ROS1 kinase domain resulting in resistance to crizotinib in a woman with metastatic lung adenocarcinoma.
Crizotinib is an oral ATP-competitive selective  inhibitor of the anaplastic lymphoma kinase (ALK) and MET tyrosine kinase that inhibits tyrosine phosphorylation of activated ALK at nanomolar concentrations. In 2011, crizotinib was approved by the U.S. Food and Drug Administration (FDA) for treatment of patients with locally advanced or metastatic non-small-cell lung cancer (NSCLC) that are ALK-positive. Activating mutations or translocations of the ALK gene have been discovered in various types of cancer, including anaplastic large-cell lymphoma, neuroblastoma, inflammatory myofibroblastic tumor, and non–small-cell lung cancer. Because of its role in lung cancer, ALK receptor tyrosine represents a potential therapeutic target.
inhibitor of the anaplastic lymphoma kinase (ALK) and MET tyrosine kinase that inhibits tyrosine phosphorylation of activated ALK at nanomolar concentrations. In 2011, crizotinib was approved by the U.S. Food and Drug Administration (FDA) for treatment of patients with locally advanced or metastatic non-small-cell lung cancer (NSCLC) that are ALK-positive. Activating mutations or translocations of the ALK gene have been discovered in various types of cancer, including anaplastic large-cell lymphoma, neuroblastoma, inflammatory myofibroblastic tumor, and non–small-cell lung cancer. Because of its role in lung cancer, ALK receptor tyrosine represents a potential therapeutic target.
In addition to ALK mutations or translocations, chromosomal rearrangements in another tyrosine kinase receptor, ROS1, was identified in a molecular subset of NSCLC with distinct clinical characteristics that are similar to those observed in patients with ALK-rearranged NSCLC. Crizotinib was found highly sensitive in lung cancer patients who harbor rearrangements in ALK or ROS1. However, resistance to crizotinib was reported in lung cancer due to secondary mutations in ALK. To overcome this problem a new compound CH5424802 has been identified and is currently in clinical trials (ClinicalTrials.gov number, NCT01588028) for ALK-positive NSCLC.
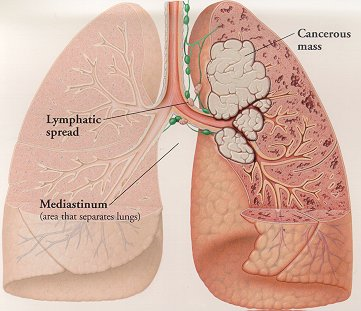
A 48-year-old woman with metastatic lung cancer and a distant history of light smoking was initially treated with first line of chemotherapy with carboplatin and pemetrexed. Genetic analysis with patient’s cancer cells showed no mutation in oncogenic KRAS or EGFR and no ALK translocations. Additional molecular testing revealed ROS1 rearrangement lead to expression of a fusion protein CD74-ROS1. After three cycles of chemotherapy, marked disease progression was noted and patient’s condition deteriorated. The patient was then enrolled in a clinical trial evaluating the safety and efficacy of crizotinib in cancer patients with ROS1 translocations (ClinicalTrials.gov number, NCT00585195). Computed tomographic scan (CT) obtained two months after treatment noted dramatic response to treatment. However, one month later, while the patient was still taking crizotinib, disease progression was observed and unfortunately the patient expired. Molecular analysis of tumor samples from all sites of disease detected a mutation glycine to arginine Gly2032Arg (G2032R) spanning CD74-ROS1 fusion area that had not been observed in pretreated samples. No other mutation of ROS1 kinase was identified by deep sequencing. Thus this suggested that appearance of G2032R mutation was an early event in crizotinib-resistant tumor cells.
To identify role of G2032R mutation in crizotinib resistance, 293T cells were transfected with either mutated or nonmutated G2032R CD74-ROS1 and subsequently treated with tyrosine kinase inhibitors crizotinib and TAE648. Cells transfected with a mutated form of ROS1 exhibited a half-maximal inhibitory concentration (IC50) value greater than 1000 nM while for nonmutated cells it was approximately 30 nM for crizotinib and 50 nM for TAE648. Crystal structure analysis of ROS1 revealed an arginine at position 2032 resulted in steric interference of crizotinib binding. Collectively, this study reported a mechanism of acquired resistance to crizotinib in a cancer driven by oncogenic ROS1 fusion. Therefore, in the context of these observations, it may be necessary to identify novel compounds that specifically target the G2032R ROS1 mutant to overcome the development of crizotinib resistance in cancers driven by ROS1.
References:

Arup Chakraborty is postdoctoral research fellow at the National Cancer Institute, Bethesda, MD. He earned a doctoral degree from Texas Tech University, and his primary research interest is in the field of clinical cancer mainly in mechanisms of resistance to molecularly targeted therapies