Several recent findings have identified variants in predominantly immune-response genes as underlying contributors in autoimmune diseases’ development. Nonetheless, along with other autoimmune disorders, there has been a significant increase particularly in incidences of multiple sclerosis (MS) and type-1 diabetes. These observations imply that in addition to the genetic causality, specific changes in environmental factors are significant contributors to the recent increases in autoimmune disorders.
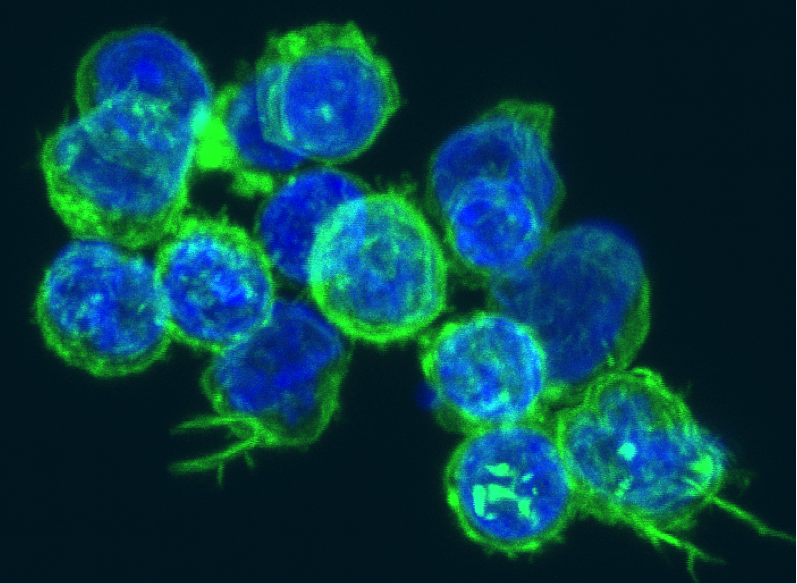
Maintenance of immune system’s homeostasis is dependent on highly specified regulation of pro-inflammatory and regulatory CD4+ helper T-cell populations. TH17 cells are pathogenic pro-inflammatory T-cells that produce a proinflammatory cytokine, Interleukin 17A (IL-17) and while they play a major role in immune defense against extracellular pathogens, they also play a major role in induction of autoimmune disorders, such as MS, psoriasis, rheumatoid arthritis, and type-1 diabetes, for which T-cell modulation is a common treatment regime.

Three previously identified factors, Interleukin 6 (IL-6), Transforming growth factor β (TGFβ) and Interleukin-23 subunit alpha (IL-23) are key players in the induction of naïve CD4+ T-cells to differentiate into TH17 cells. However, the complete mechanism and factors responsible for stimulating naïve CD4+ T-cells’ differentiation into TH17 cells is not well understood. Understanding of these underlying factors is crucial for developing therapeutic strategies to control TH17 cell differentiation.
Three complementary, collaborative studies published in Nature this week report compelling insights on the regulatory mechanism of TH17 cell differentiation and subsequent inflammatory response, while revealing evidence of interplay of genetics and a new environmental factor involved in autoimmune disease susceptibility.
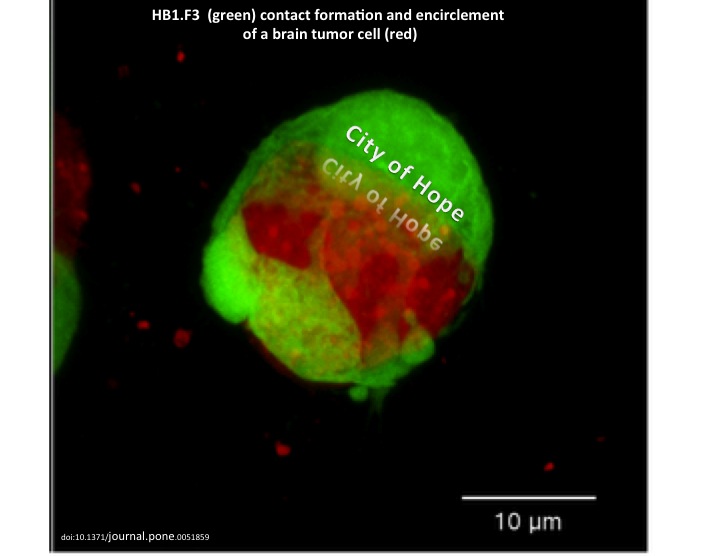
By utilizing a unique approach, consisting of combination of transcriptional profiling, novel computational methods and nanowire-based short interfering RNA (siRNA) delivery to construct, Regev’s group was able to and identify 12 novel regulators and decipher the complex transcriptional network of TH17 differentiation; they found that TH17 differentiation is regulated by two intra-connected, but antagonistic networks, such that one module promotes TH17 differentiation and proliferation while suppressing the development of other T-cells, whereas the antagonist module suppresses TH17 cells.
By upregulating the expression of IL-23 receptor (IL-23R) on TH17 cells, IL-23 sustains the TH17 inflammatory response and induces its pathogenic effector functions. Through transcriptional profiling, Kuchroo’s group found that a serine/threonine kinase, Serine/threonine-protein kinase 1 (SGK1), an essential node downstream of IL-23 signaling, is crucial for regulating IL-23R expression and stabilizing the TH17 cell pathogenic effector function by inhibiting the molecule that represses IL-23R expression.
Previous studies have shown that SGK1 regulates Na+ transport and NaCl (salt) homeostasis in cells. Interestingly, Kuchroo’s study shows the positive correlation between increased concentration in salt and SGK1 expression, followed by upregulation of IL-23R and enhanced TH17 differentiation in vitro as well as in vivo.
Consistent with Kuchroo’s finding, Hafler’s group reported that excess NaCl uptake can affect the innate immune system, and provided compelling data suggesting the possibility of the direct positive correlation between increased salt intake and incidence of autoimmune disease.
Previous studies have suggested the involvement of environmental factors, such as viruses, smoking, lack of sunlight and Vitamin D in different autoimmune disorders. Salt, as the new potential environmental factor in autoimmune diseases is certainly an intriguing notion; not only due to the relevant molecular mechanisms reported in the three new studies, but also due to the fact that in most developed countries, the consumption of processed foods (such as fast foods), which contain over 100 times more NaCl compared to non-processed meals, has increased significantly over the past three decades. Nonetheless, future epidemiological studies in humans are needed to further investigate the possible correlation between salt consumption and autoimmunity incidence.
Further Readings:
Induction of Pathogenic TH17 Cells by Inducible Salt-sensing Kinase SGK1
Dynamic Regulatory Network Controlling TH17 Cell Differentiation
Sodium Chloride Drives Autoimmune Disease by The Induction Of Pathogenic TH17 Cells













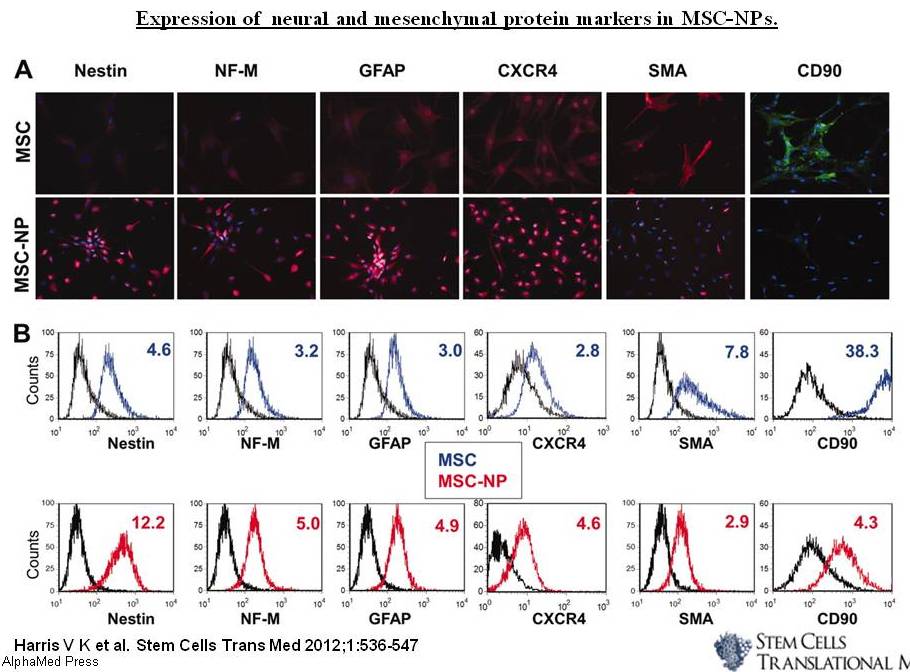

 536-47, Figure 3.jpg)